With new COVID lockdowns in place for Greater Sydney and community sport taking a 2 week break, we often see these types of unscheduled breaks lead to injuries when sport resumes.
Planning ahead and implementing some strategies for injury prevention will help you navigate the lockdown break and keep you on the pitch for longer.
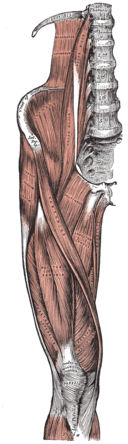
Hamstring injuries are common amongst professional footballers and Sunday afternoon superstars alike.
Some research into hamstring injuries has demonstrated that if the hamstring musculature is strong and flexible as opposed to weak and short then it significantly decreases the risk of hamstring injury throughout the course of a season (Timmins et al. 2016 and Bourne et al. 2018).
The Quadrant of Doom
Below is an infographic from YLM Sports Science that clearly demonstrates the relationship between strength, flexibility and injury risk. The other way to frame this is in terms of capacity. The greater the strength and movement capacity then the less likely things are to go wrong.
The other benefit from all of the below is that by incorporating this it will not decrease injury risk but also improve performance!
Knowing this is all well and good but we also want to practically act on this. How do we build things up from a loading, flexibility and strength point of view. Below is another great infographic from YLM Sports Science that shows specific ways to address all these areas.
In summary to build strong, functional and flexible hamstrings then it is worth looking at an exercise program that includes hip and knee dominant exercises that is gradually overloaded to create adaptation. It is also worth adding some running and sprint work into the program as this is shown to have a protective effect and also some loaded flexibility work to strengthen the hamstrings in lengthened positions (Oakley et al.2018).
Take Home points for hamstring performance and health:
Strong and long hamstrings are the goal
Use knee and hip dominant strengthening exercises
Incorporate sprint work
Work on flexibility
Progressively overload
Stay consistent
References:
Timmins RG, Bourne MN, Shield AJ, et al. Short biceps femoris fascicles and eccentric knee flexor weakness increase the risk of hamstring injury in elite football (soccer): a prospective cohort study. Br J Sports Med 2016;50:1524-1535. https://bjsm.bmj.com/content/50/24/1524
Bourne, Matthew N., Timmins, Ryan, Opar, David A., Pizzari, Tania, Ruddy, Joshua, Sims, Casey, WIlliams, Morgan, & Shield, Anthony (2018) An evidence-based framework for strengthening exercises to prevent hamstring injury. Sports Medicine, 48(2), pp. 251-267. https://link.springer.com/article/10.1007/s40279-017-0796-xhttps://ylmsportscience.com/
2017/11/26/hamstring-strain-injury-escape-the-quadrant-of-doom/
Oakley AJ, Jennings J, Bishop CJ. Holistic hamstring health: not just the Nordic hamstring exercise. Br J Sports Med 2018;52:816-817. https://bjsm.bmj.com/content/52/13/816