We know the feeling. You’ve been training solidly, competing well and things feel like they’re coming together (finally!).
Until that moment amongst a heated roll, that you lose your base and land smack-bang on the point of your shoulder.
You have an immediate reflexive wince of pain. You feel like someone stuck a knife into the point of your shoulder and your arm ain’t moving very far away from your body.
It definitely doesn’t like you moving the arm across the body and it may even look like a little speed hump at the end of your shoulder.
Welcome to the acromioclavicular joint, the notorious AC joint in contact sports like BJJ. This is the joint that lies between the end of your collarbone and shoulder blade and acts as a strut to stabilise the shoulder/arm complex.
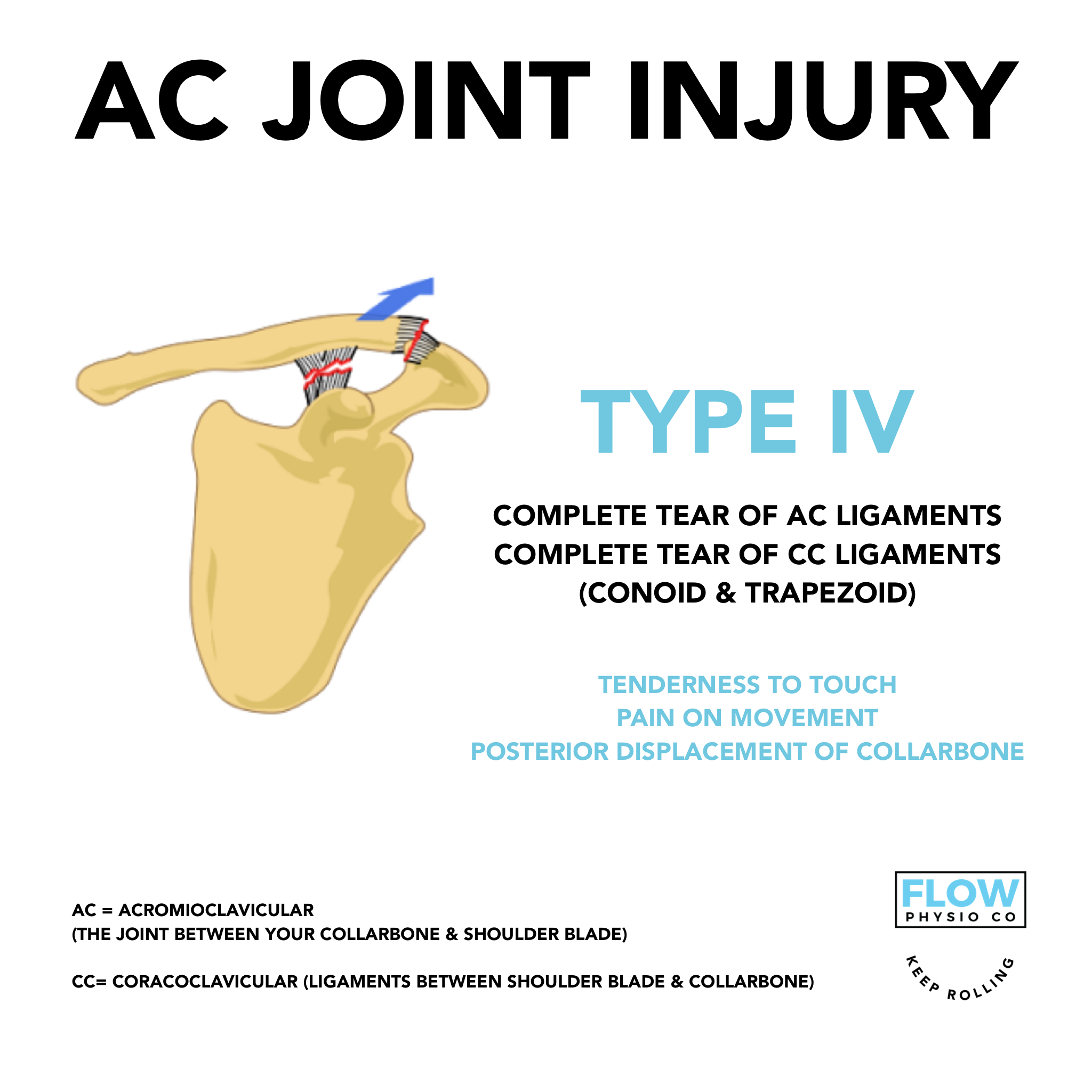
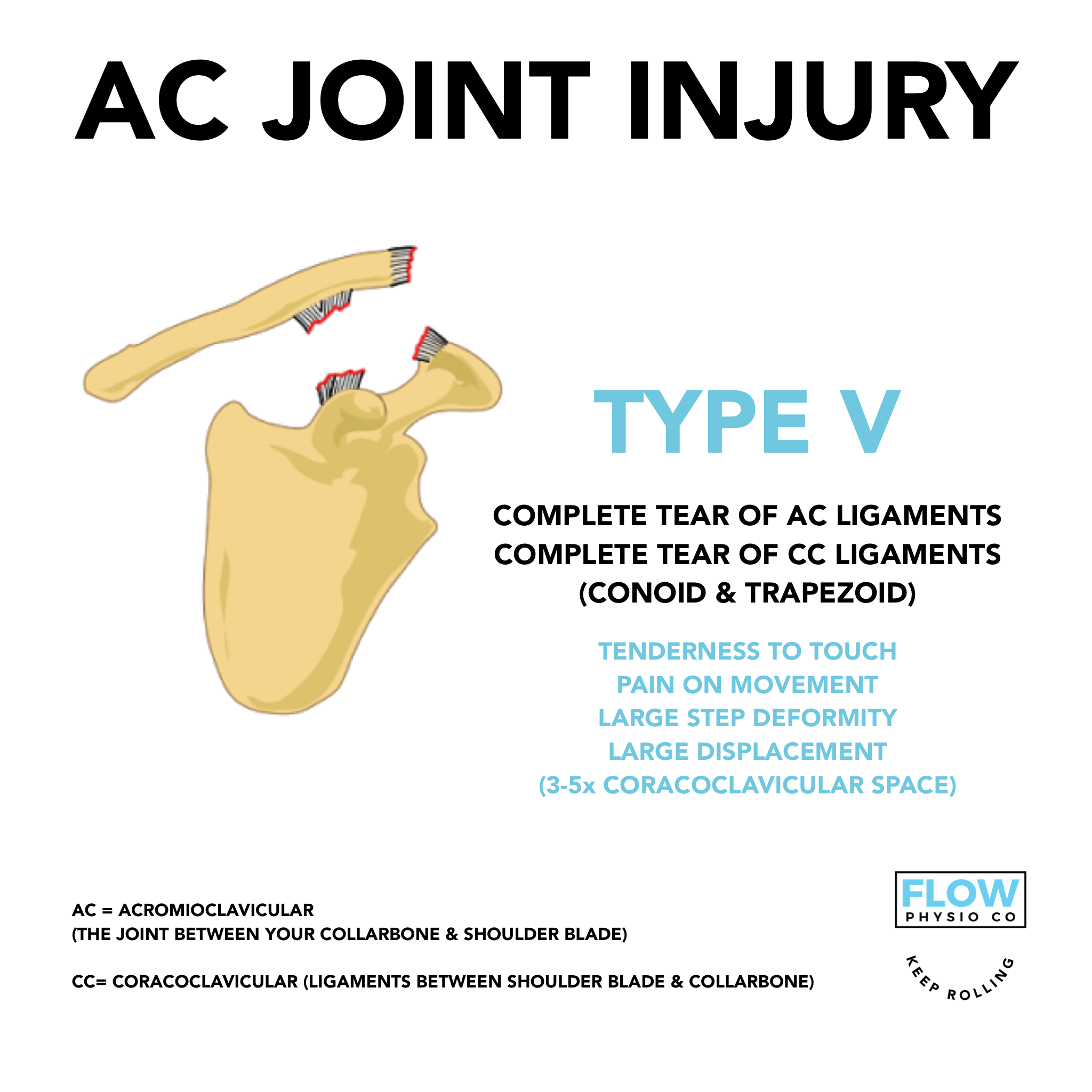
These AC joint injuries are classified into 6 different types according to the commonly used Rockwood Classification:
DO I NEED SURGERY?
Management of AC joint injuries follows the general principles of all ligament injuries and will be dependant on the grade (type) and the end goals of the individual.
As a general rule, surgical intervention may be indicated for type 4, 5 and 6 AC joint injuries and type 3 injuries that do not respond to non-surgical management.
Low grade AC Joint injury - what now?
Like all injuries, the rehabilitation and exercise or loading exposure will vary from person-to-person. As a general guide, initial management begins immediately and aims to minimise bleeding and swelling and treatment aims to:
promote tissue healing
prevent stiffness
protect from further damage
strengthen shoulder musculature to provide dynamic stability.
Isometric strengthening exercises can be started as soon as pain allows and usually begin close to the body with a progression plan to move away from the body as the body undergoes it’s natural healing response to injury.
When can i return to sport? When can I roll again?
We usually look for no AC joint tenderness and full pain-free movement as a starting point for starting the conversation about returning to sport.
We like to see the completion of a full rehabilitation program that focuses on restoring full function and strength of the entire shoulder complex, as well as a graded return to rolling that may involve light drilling and flow rolls initially, with an increase in exposure as the shoulder adapts to the additional stress loads of training.
Full return to training will be individual-specific and criteria driven.
Keep Rolling!